The most obvious symptom of the NHS crisis is Accident and Emergency (A&E). Less than 68% of people were assessed, treated, admitted or discharged within the Scottish Government’s four-hour A&E target. More than 6,800 people spent more than 12 hours in A&E in October. While there is much in the Scottish Futures report to agree with, including patient-centred care, more volunteers doesn’t hack it. While the different NHS systems in the UK should cooperate, their emphasis on this is more political than practical. NHS Scotland is big enough to operate mainly on its own. More UK bureaucracy won't help.
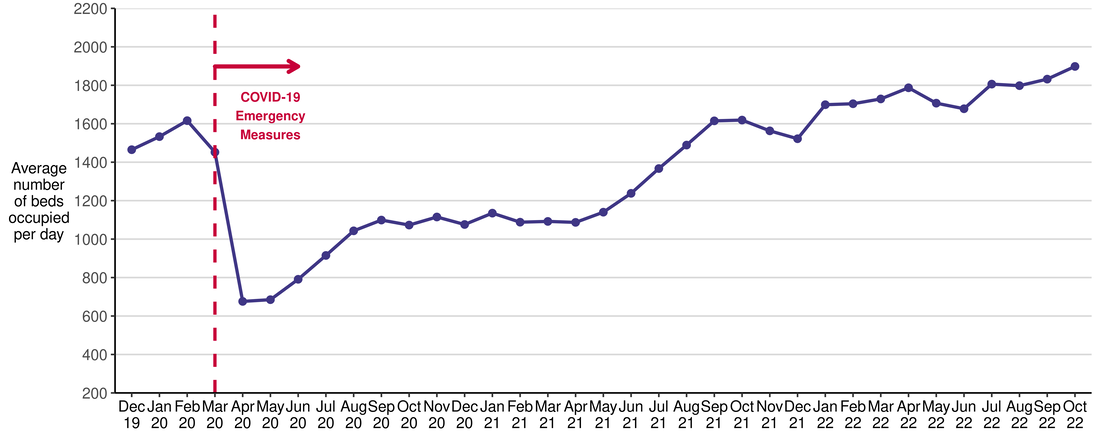
The latest NHS Scotland delayed discharge statistics illustrate the need to focus on social care. A delayed discharge occurs when a hospital patient who is clinically ready for discharge from inpatient hospital care continues to occupy a hospital bed beyond the date they are ready for discharge. In October 2022, the average number of beds occupied per day due to delayed discharges was 1,898, the highest figure since the current guidance came into place in July 2016. To put this number in context, the Queen Elizabeth University Hospital in Glasgow has 1677 beds. So, delayed discharge is the equivalent of our largest hospital and then some. The chart below shows this is not a short-term blip.
The latest care inspectorate statistics showed that 60% of care services that employ nurses reported vacancies, creating a 16% vacancy rate. The staffing issues are not limited to social care. NHS district nurses play a crucial role in supporting people to return home from hospital. The vacancy rate for district nursing reached 16% last month. The Westminster Adult Social Committee has highlighted similar concerns in England.
The idea that more privatisation is the solution is risible. As Prem Sikka recently highlighted, social care companies are robbing the public purse, with profit margins of between 37% and 41.7%, and tax dodging is rife. This is the model that people like Karol Sikora want to expand! In addition, self-funding care home residents are now paying 40% more than publicly-funded residents, compared with 24% a decade ago.
Sadly, the proposed National Care Service in Scotland will do nothing to challenge this, taking even more services from the public sector. Moreover, as the Scottish Parliament Finance Committee report highlighted, the costings of this over-centralised service are largely unknown. Still, we do know that it will divert much-needed resources from frontline services. Creating a National Care Service remains the right approach. However, its role should be to create a national framework, with services designed and delivered locally. Implementing organisational change of this magnitude will take a significant amount of time. In the meantime, we need to support the demoralised, tired, and financially stretched frontline staff who immediately need a break, decent pay and a vote of confidence.
There has been a welcome initiative from former health ministers Alex Neil and Malcolm Chisholm to end zero-hours contracts. However, the response from Social Care Minister Kevin Stewart that companies bidding for government work are evaluated on their fair working practices "where it is relevant and proportionate to do so" - is not good enough.
Patients overwhelmingly access the NHS through GP services. However, patient surveys show this is becoming increasingly difficult despite GPs delivering more appointments (not all in person) than before the pandemic. Patient satisfaction is 12% down in the last year, with 10% saying it had become more difficult even to contact their GP practice. Some of the byzantine appointment systems don't help and put excessive pressure on reception staff, who take the brunt of patient dissatisfaction.
This is primarily an issue for non-urgent treatment; charging better-off patients won’t help address this. While it may discourage some appointments, this short-term gain will result in long-term pain as conditions go undiagnosed, resulting in more severe conditions for the NHS to treat. The solution is recruiting more GPs and other health staff in primary care. GP numbers have fallen from 3,613 in 2019 to 3,494 in 2022. Scottish Government targets focus on headcount, which ignores the growing number of part-time staff. A BMA Scotland survey indicated that 75% are more likely to quit or reduce hours in the coming year due to ‘excessive workload’. Five years on, the deployment of multi-disciplinary teams has fallen short because of staffing shortages.
Moving away from the expensive small-business model would also help in the longer term. Many more GPs, particularly younger staff, are coming to this view. For example, GPs at the Lothian LMC have recently said that the independent contractor model ‘is no longer fit for purpose.’
The NHS as an institution rightly attracts almost universal support, primarily because we all rely on it. That doesn't mean it is sacrosanct, and it is perfectly reasonable to debate reform. However, we must be wary of those who use reform as a trojan horse to promote their ideological agenda. The founding principles of an NHS free at the point of need, funded by general taxation, is the best way to organise healthcare. The NHS's main problem is the absence of adequately funded social care and primary care. That should be our focus right now. Anything else is a distraction.

 RSS Feed
RSS Feed